Ibb Governorate, Yemen – Kholoud, 28, has known mental trauma almost all her life.
At six years of age, when Kholoud’s father married for the second time, the step mother would deprive Kholoud and her seven siblings of food, physically and verbally abuse them for no apparent reason.
“Despite the abused I endured every day, I was determined to go to school and complete my education. When I finished high school, I pleaded with my father to allow me to study midwifery. He reluctantly agreed in spite of my stepmother’s dissuasion.”
“I wanted to be a midwife. Midwives are respected. I thought being a midwife would give me the freedom to help and guide other women to have fulfilling lives,” Kholoud tells UNFPA.
When Kholoud completed her degree, a man offered his hand in marriage. She was 17 years of age when she married.
“I knew nothing about him, but I agreed without hesitation to escape home, which was a tormenting my mental health,” tells Kholoud.
Three years into their marriage, the conflict in Yemen erupted, shutting down the health facility Kholoud was working in – nearly 50 per cent of health facilities have remained closed since the escalation of the conflict in Yemen.
Her husband also lost his job. With no income, their living conditions became dire and anxiety levels rose with no food to feed their three children
“My husband started to exploit me. He took all my money and possessions and sold them to open a small clinic for me in the village. He forced me to work day and night and kept pressurizing me to make more money. I completely burnt out.
Kholoud returned to her father in desperation. Seeing her mental state, he took her to Taizz to seek treatment. The cost of the treatment and travel was too much for her father to bare, Kholoud had to stop the treatment half way.
Mental health needs soar as the conflict deepens
An estimated one in five people suffer from mental health disorders, according to a 2017 study conducted by the Family Counselling and Development Foundation. This number is likely to have increased due to the COVID-19 pandemic and over eight years of conflict.
Mental health services remain scarce. There are only 46 psychiatrists across the country making it one of the worst worldwide in terms of the number of psychiatrists per population, with 1 psychiatrist for every 700,000 people. Some of the few existing mental health services have even closed as a result of the COVID-19 pandemic.
In 2023, some 7 million people are estimated to require mental health treatment and support, but only 120,000 have uninterrupted access to these services
A cycle of abuse
Kholoud’s mental health improved despite the interruption in treatment, until her husband came back, demanding for her return to the village. He continued to physically and verbally abuse her and her children until she agreed to return to prevent further abuse of her children.
Kholoud was forced to work at the clinic once again. She agreed to his demands to stop him from physically abusing the children if she didn’t work and provide him money.
“The constant exploitation and humiliation broke me. I ended up worse than before,” adds Kholoud.
This time Kholoud reached out to her sister, who took her to her home. Her father could no longer afford to help without a source of income.
Kholoud stayed with her sister for over two months in severe mental trauma, waiting for help.
Her sister heard about a hotline offering mental health services on the radio, and called immediately and booked an appointment for the next day.
Repairing mental health and wellbeing
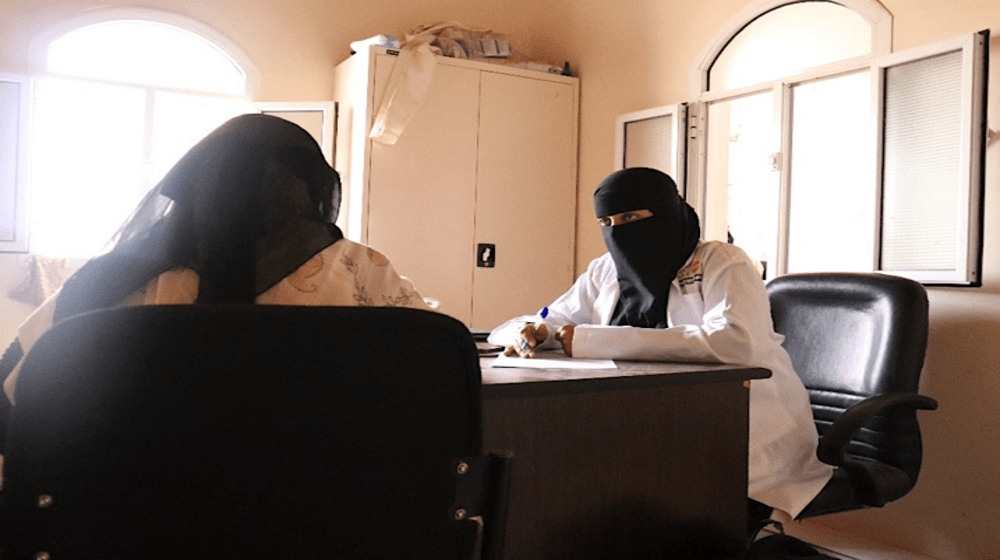
When Kholoud arrived at a UNFPA-supported specialized mental health care centre in Ibb, funded by the European Union Humanitarian Aid, she was immediately referred to a psychiatrist, and provided with medications free of charge. Here treatment continued for five months, until she fully recovered.
In addition, Kholoud was referred to a UNFPA-supported women and girls safe space that provided legal support to obtain a divorce and take custody of her children.
“When you lose all hope and the will to live and waiting for death, suddenly relief comes to you, this is how the mental health centre has saved me,” tells Kholoud.
Now Kholoud has rented a small house for herself and her children close to her sister and is working in a nearby hospital that the mental health centre helped to find for Kholoud.
“I am repairing the mental wellbeing of myself and my children, free from exploitation, abuse and exhaustion. People appreciate my work and respect me, this is why I wanted to be a midwife. I am finally getting exactly what I deserve,” states Kholoud.
UNFPA’s response
In June 2018, UNFPA’s supported the establishment of two psychological care centres entitled Family Counseling Centres in Sana’a and Aden Governorates, to reduce and mitigate psychological effects of GBV survivors and provide specialized multi-level mental health services to GBV survivors in targeted as well as neighboring governorates.
At present six such psychological care centres are being supported by UNFPA in the governorates of Aden, Taizz, Ibb and Sana’a with funding from Canada, European Union Humanitarian Aid, Norway and USAID’s Bureau for Humanitarian Assistance.
Since the beginning of 2023, nearly 100,000 people have been received specialized psychological support through the hotline and in person at these centres, over three quarters of them being survivors of gender-based violence.